More babies in England could die from issues caused by unlicensed medicines if providers are not required to report problems, a coroner has warned.
The conclusions were reached at the end of an inquest held after three infants died due to receiving contaminated feed.
The babies were all receiving hospital care after being born prematurely and died after receiving total parenteral nutrition (TPN) feed contaminated with Bacillus cereus, Southwark coroners court heard.
Three-month-old Aviva Otte, one-month-old Oscar Barker and nine-day-old Yousef Al-Kharboush were being provided critical nutrition via TPN. Aviva’s mother, Jedidajah Otte, is a Guardian journalist.
Otte has spoken previously of how she encountered a “stubborn refusal” by doctors and nurses at St Thomas’ hospital in London to tell her what was happening with Aviva’s health.
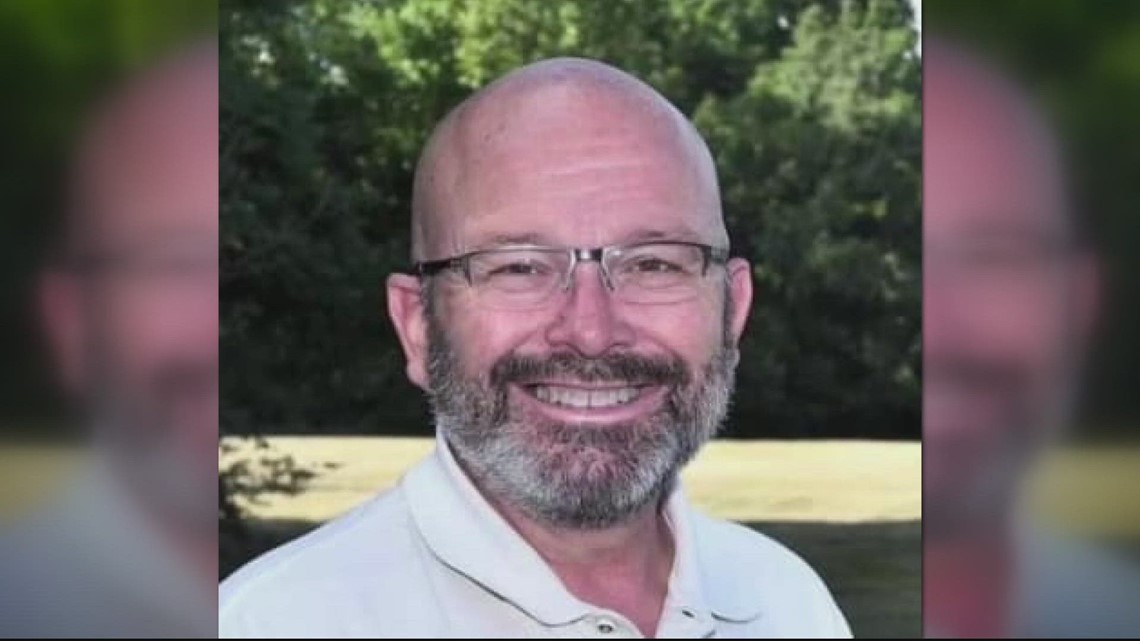
Aviva died in January 2014 at St Thomas’ and received TPN “provided and compounded” by the NHS establishment under a section 10 exemption, according to a preventing future deaths (PFD) report by the senior coroner, Dr Julian Morris.
The exemption under the Medicines Act 1968 allows organisations to legally produce bespoke medicines without a licence for specific patients facing niche problems.
Yousef, who in June 2014 also died at St Thomas’, and Oscar, who died at Addenbrooke’s hospital in Cambridge the same month, received TPN produced by a “commercial provider” – ITH Pharma, which is a licensed provider and not subject to the section 10 exemption.
In his report, Morris highlighted concerns about what obligations section 10 exempt entities are under to report “adverse events”. He said: “There is no requirement for a section 10 exempt entity to report any of its findings to the MHRA [Medicines and Healthcare products Regulatory Agency] or indeed to other trusts or the industry in general if an adverse event occurs.
“The current reporting structures [for a section 10 entity] involve reporting to NHSE and the CQC but the threshold or necessity for such reporting appears unclear and, in essence, up to the trust.
“There may be times when section 10 entities reach conclusions which would assist the wider industry and help to assist both other trusts and commercial organisations in assessing their own risks and improving the provision of highly specific medication to a group of vulnerable patients.”
He also wrote that Bacillus cereus was resistant to some cleaning methods and that “sporocides” could be required to achieve decontamination. “This was information and a conclusion that the trust had reached in early 2014 and therefore prior to the outbreak in May-June 2014,” Morris said.
There was a risk that future deaths could occur unless action was taken in respect of the highlighted concerns.
Recipients have to respond to the report by 8 January.
ITH Pharma was fined £1.2m by a crown court in 2022 after providing TPN from which 19 premature babies became infected across nine hospitals in 2014. The company pleaded guilty to a single regulatory offence of failing to have a suitable and sufficient risk assessment, under the management of health and safety at work regulations 1999, and to two regulatory offences under the Medicines Act 1968 of supplying a medicinal product on 27 May 2014 not of the nature or quality specified in the prescription
An ITH Pharma spokesperson said: “Any information that had been shared with ITH and the MHRA as a result of a previous outbreak in the NHS five months prior to the ITH incident could have been of real value in taking steps to prevent future possible incidents.
“We are proud to work with and support the NHS and importantly, patients in this vital work of specialised feeding systems. We offer our deepest sympathies to all the families affected by the events of 10 years ago.
“We have done everything possible to assist the senior coroner in ensuring these inquests examined the full picture of both outbreaks in 2014 and we hope that these findings provide the families with answers.”
.png)
 3 hours ago
1
3 hours ago
1








 English (US) ·
English (US) ·